Hemodialysis
Increased dialysis effectiveness with MOTOmed Movement Therapy
Due to a significantly increased cardiovascular risk, dialysis patients have only 17 % to 39 % depending on their age of the life expectancy compared to the normal population. Scientific studies show that structured, performance-controlled training with MOTOmed Movement Therapy is feasible during dialysis. The increase in strength and endurance achieved and the consequent increase in performance can improve quality of life and reduce morbidity.
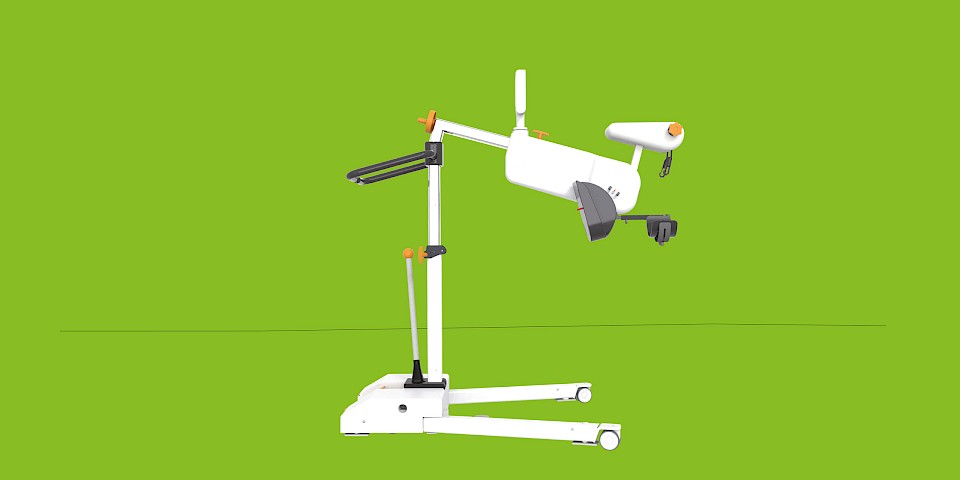
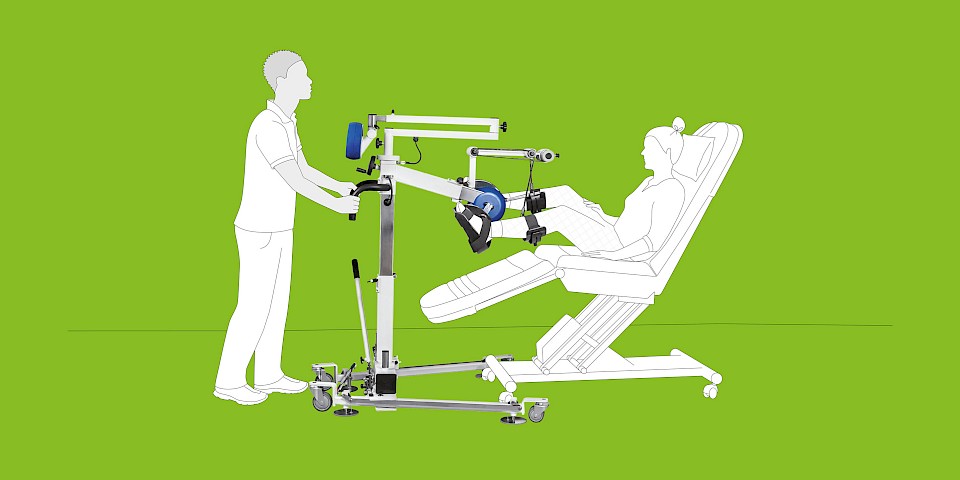
With the MOTOmed layson edition, dialysis patients can train their lower extremities individually and adapted to their personal performance from bed or from the dialysis couch. The patient‘s legs are safely supported. Even weak, multimorbid patients benefit from MOTOmed Movement Therapy in supine position thanks to the three therapy modes - passive (letting oneself be moved), assistive (motor-assisted) or active (using one‘s own muscle power).
Scientific study
Dziubek W, Bulińska K, Rogowski Ƚ, Kusztal M. Three-month endurance training improves functional fitness and knee muscle performance of patients with end stage renal disease (ESRD). Isokinetics and Exercise Science 24 (2016); 237 – 246.
Configure your personal MOTOmed
Use the MOTOmed Product Configurator to configure your MOTOmed according to your requirements. Quickly, easily and without obligation. Try it out and configure your personal and individualized MOTOmed now.
MOTOmed Movement Therapy
MOTOmed Movement Therapy was developed for people with movement restrictions and complements physical, ergo and sports therapy measures. Patients in supine position use MOTOmed from a nursing bed or therapy couch.
In Germany, the device-based movement therapy with the MOTOmed is recognized as an aid for many indications by the statutory health insurance. It is worthwhile to inform yourself!
Therapy modes
passive
The effortless motor driven movement is ideal for the regulation of muscle tone, loosening stiff muscles and for early mobilization after long rests. Passive training stimulates blood circulation, digestion and joint flexibility.
assistive
In motor-supported movement therapy, the function MOTOmed ServoCycling enables easy transition from passive to active training. A motor-supported movement stimulates strength and endurance even with minimal muscle strength.
active
An active training with own muscle power against finely adjustable resistance levels strengthens leg, arm and upper body muscles and stimulates the cardio-vascular system.
Achieving best therapy goals through interval training
Alternating phases of strain and recreation (intervals) through active and passive training give a higher training stimulus which leads to a better therapy success.
Therapeutic goals
- Promote walking
- Reduce the consequences of lack of movement
- Activate residual muscle strength
- Strengthen the psyche and well-being
- Counteract fatigue
MOTOmed layson.l presentation
Videos
Scientific studies and research results about the MOTOmed movement therapy during hemodialysis
7.6) Anding-Rost K., von Gersdorff G., von Korn P., Ihorst G., Josef A., Kaufmann M., Huber M., Bär T., Zeißler S., Höfling S., Breuer C., Gärtner N., Haykowsky M.J., Degenhardt S., Wanner C., Halle M. (2023). Exercise during Hemodialysis in Patients with Chronic Kidney Failure. NEJM Evidence, EVIDoa2300057., DOI: 10.1056/EVIDoa2300057
7.5) Mitsiou M., Dimitros E., Roumeliotis S., Liakopoulos V., Kouidi E., Deligiannis A. (2022). Effects of a Combined Intradialytic Exercise Training Program and Music on Cardiac Autonomic Nervous System Activity in Hemodialysis Patients. Life, 12(8), 1276., DOI: 10.3390/life12081276
7.4) Dziubek W., Bulińska K., Rogowski Ƚ., Kusztal M., Zembroń-Ƚacny A., Goƚȩbiowski T., Markowska D., Klinger M., Woźniewski M. (2016). Three-month endurance training improves functional fitness and knee muscle performance of patients with end stage renal disease (ESRD). Isokinetics and Exercise Science, 24(3), 237-246., DOI: 10.3233/IES-160623
7.3) Dziubek W., Kowalska J., Kusztal M., Rogowski Ƚ., Gołębiowski T., Nikifur M., Szczepańska-Gieracha J., Zembroń- Łacny A., Klinger M., Woźniewski M. (2016). The Level of Anxiety and Depression in Dialysis Patients Undertaking Regular Physical Exercise Training – a Preliminary Study. Kidney Blood Pressure Research, 41(1), 86–98., DOI: 10.1159/000368548
7.2) Anding K., Bär T., Trojniak-Hennig J., Kuchinke S., Krause R., Rost J.M., Halle M. (2015). A structured exercise program during haemodialysis for patients with chronic kidney disease: clinical benefit and long-term adherence. BMJ Open, 5(8)., DOI: 10.1136/bmjopen-2015-008709
7.1) Torkington M., MacRae M., Isles C. (2006). Uptake of and adherence to exercise during hospital haemodialysis. Physiotherapie, 92(2), 83-87., DOI: 10.1016/j.physio.2005.08.004