Intensive care / Early Mobilisation
Improvement of rehabilitation and quality of life of intensive care patients
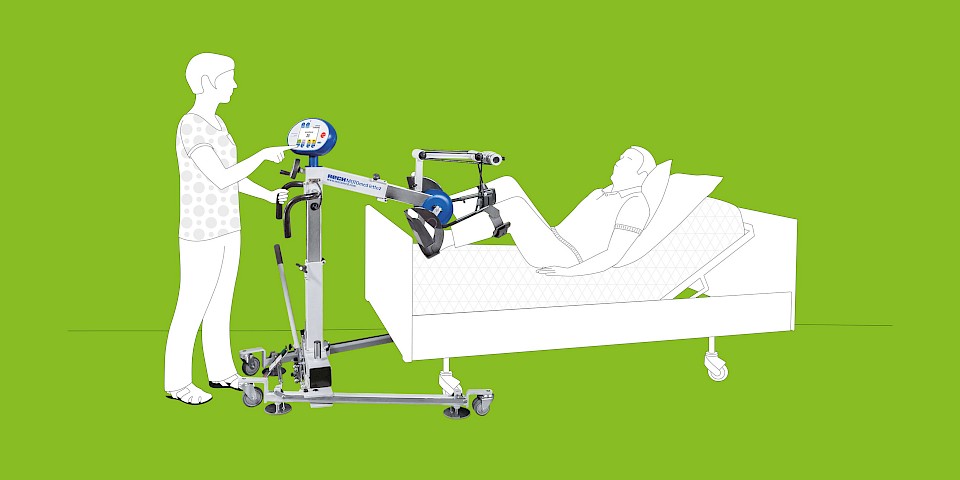
Mobilization as early as possible is the basis for a successful rehabilitation process and in many cases leads to an earlier transfer from the intensive care unit and subsequent discharge from the hospital. Scientists are currently working on the development of standards and guidelines for early mobilization. In this context, the motor-driven MOTOmed Movement Therapy in supine position plays a major role.
With regular use, joint mobility can be maintained and blood circulation and metabolism can be activated. In addition, MOTOmed Movement Therapy represents a natural decubitus and thrombosis prophylaxis. Initial scientific findings also indicate earlier weaning from ventilation (weaning) through the use of MOTOmed Movement Therapy in supine position.
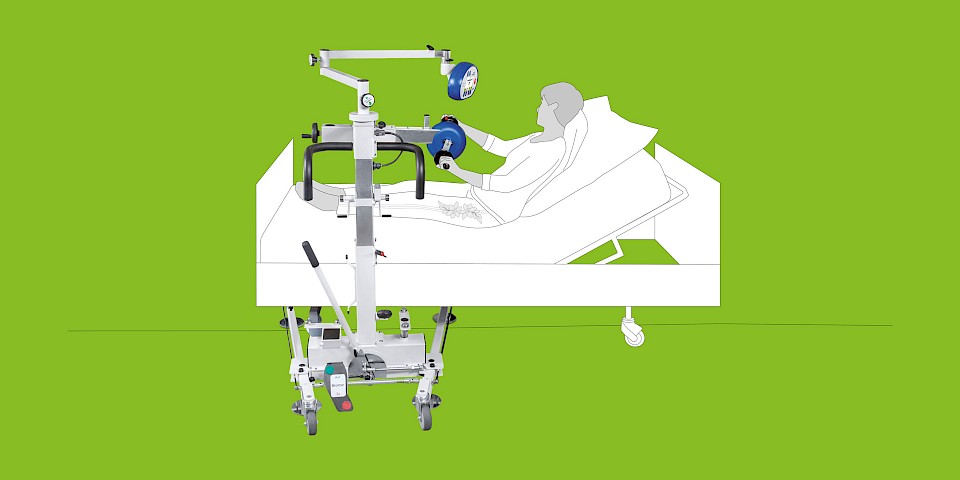
The use of a MOTOmed layson edition model enables a recumbent, possibly comatose person in the intensive care unit a safe form of passive mobilization. In addition, the „ServoCycling“ therapy aid can be used while the patient is awake to provide assistive training adapted to the patient‘s condition, even with minimal muscle strength. This leads to a considerable increase in motivation and consent to further rehabilitation.
The intuitive handling and the user-friendly operation via touch screen enables therapists and nursing staff to use the MOTOmed layson edition very easily.
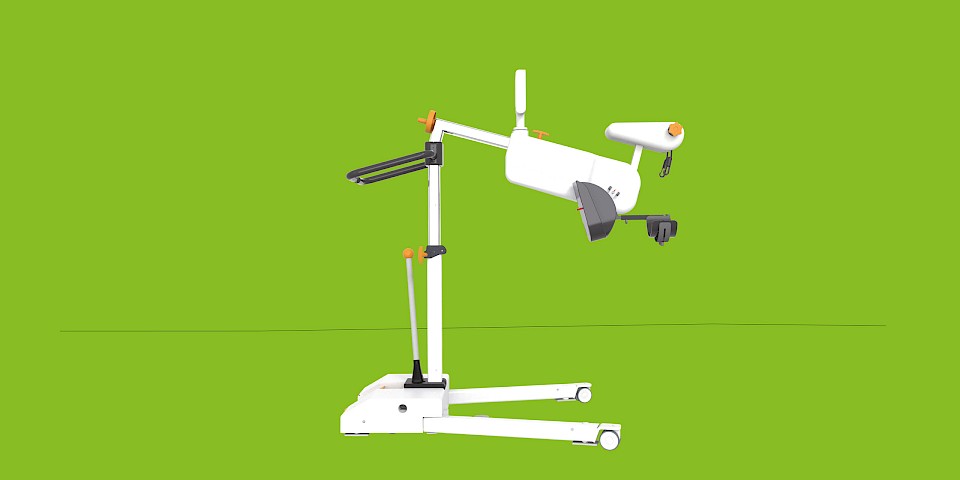
Configure your personal MOTOmed
Use the MOTOmed Product Configurator to configure your MOTOmed according to your requirements. Quickly, easily and without obligation. Try it out and configure your personal and individualized MOTOmed now.
MOTOmed Movement Therapy
MOTOmed Movement Therapy was developed for people with movement restrictions and complements physical, ergo and sports therapy measures. Patients in supine position use MOTOmed from a nursing bed or therapy couch.
In Germany, the device-based movement therapy with the MOTOmed is recognized as an aid for many indications by the statutory health insurance. It is worthwhile to inform yourself!
Therapy modes
passive
The effortless motor driven movement is ideal for the regulation of muscle tone, loosening stiff muscles and for early mobilization after long rests. Passive training stimulates blood circulation, digestion and joint flexibility.
assistive
In motor-supported movement therapy, the function MOTOmed ServoCycling enables easy transition from passive to active training. A motor-supported movement stimulates strength and endurance even with minimal muscle strength.
active
An active training with own muscle power against finely adjustable resistance levels strengthens leg, arm and upper body muscles and stimulates the cardio-vascular system.
Achieving best therapy goals through interval training
Alternating phases of strain and recreation (intervals) through active and passive training give a higher training stimulus which leads to a better therapy success.
Therapeutic goals
- Promote walking
- Reduce the consequences of lack of movement
- Reduce spasticity
- Activate residual muscle strength
- Strengthen the psyche and well-being
- Counteract fatigue
MOTOmed layson.l presentation
Videos
Scientific study about MOTOmed movement therapy in bed-ridden patients
8.10) Hickmann C.E., Montecinos-Munoz N.R., Castanares-Zapatero D., Arriagada-Garrido R.S., Jeria-Blanco U., Gizzatullin T., Roeseler J., Dugernier J., Wittebole X., Laterre P.-F. (2021). Acute effects of sitting out of bed and exercise on lung aeration and oxygenation in critically ill subjects. Respiratory care, 66(2), 253-262., DOI: 10.4187/respcare.07487
8.9) Nickels M.R., Aitken L.M., Barnett A.G., Walsham J., McPhail S.M.Publish (2020). Acceptability, safety, and feasibility of in-bed cycling with critically ill patients. Australian Critical Care, 33(3), 236-243., DOI: 10.1016/j.aucc.2020.02.007
Yu L., Jiang J.-X., Zhang Y., Chen Y.-Z., Shi Y. (2020). Use of in-bed cycling combined with passive joint activity in acute respiratory failure patients receiving mechanical ventilation. Annals of Palliative Medicine, 9 (2), 175-181., DOI: 10.21037/apm.2020.02.12, DOI: 10.21037/apm.2020.02.12
8.7) Sommers J., Klooster E., Zoethout S.B., van den Oever H.L.A., Nollet F., Tepaske R., Horn J., Engelbert R.H.H., van der Schaaf M. (2019). Feasibility of Exercise Testing in Patients Who Are Critically Ill: A Prospective, Observational Multicenter Study. Archives of physical medicine and rehabilitation, 100(2), 239-246, DOI: 10.1016/j.apmr.2018.07.430
8.6) De Beer C., Van Rooijen A., Pretorius J., Becker P., Rheeder P., Paruk F. (2018). Muscle strength and endurance to predict successful extubation in mechanically ventilated patients: A pilot study evaluating the utility of upper-limb muscle strength and ergometry. Southern African Journal of Critical Care, 34(2), 44-51., DOI: 10.7196/SAJCC.2018.v34i2.360
8.5) Hickmann C., Castanares-Zapatero D., Deldicque L., Van den Bergh P., Caty G., Robert A., Roesler J., Francaux M., Laterre P.-F. (2018). Impact of Very Early Therapy During Septic Shock on Skeletal Muscle: A Randomized Controlled Trial. Critical Care Medicine., DOI: 10.1097/CCM.0000000000003263
8.4) Dos Santos Machado A., Pires-Neto R.C., Ximenes Carvalho M.T., Soares J.C., Cardoso D.M., Martins de Albuquerque I. (2017). Effects that passive cycling exercise have on muscle strength, duration of mechanical ventilation, and length of hospital stay in critically ill patients: a randomized clinical trial. Jornal brasileiro de pneumologia, 43(02), 134-139., DOI: 10.1590/S1806-37562016000000170
8.3) Schaller S., Anstey M., Blobner M., Edrich T., Grabitz S., Gradwohl-Matis I., Heim M., Houle T., Kurth T., Latronico N., Lee J., Meyer M., Peponis T., Talmor D., Velmahos G., Waak K., Walz J., Zafonte R., Eikermann M. (2016). Early, goal-directed mobilization in the surgical intensive care unit: a randomised controlled trial. The Lancet, 388 (10052), 1377-88., DOI: 10.1016/S0140-6736(16)31637-3
8.2) Kho M. E., Martin R. A., Toonstra A. L., Zanni J.M., Mantheiy E.C., Nelliot A., Needham D.M. (2015). Feasibility and safety of in-bed cycling for physical rehabilitation in the intensive care unit (ICU). Journal of Critical Care, 30(6), 1419., DOI: 10.1016/j.jcrc.2015.07.025
8.1) Burtin C., Clerckx B., Robbeets C., Ferdinande P., Langer D., Troosters T., Hermans G., Decramer M., Gosselink R. (2009). Early exercise in critically ill patients enhances short-term functional recovery. Critical Care Medicine, 37(9), 2499-2505., DOI: 10.1097/CCM.0b013e3181a38937